By Physio Team
Appointments & Fees, Exercises, Home exercises, Lockdown, online consultations, Physio, Pilates & Exercise Classes, Sporting, Studies, Therapy, Uncategorized
#physio, #physiotherapy, Blog, evidence based, exercise, Physio, physiotherapy, rehabilitation
Our daily routine has been forced to change during the lockdown and it has never been more important to focus on your physical and mental health. The current situation we’re facing is strange, stressful, emotionally exhausting and there is no surprise that the motivation to keep fit has been a bit of a struggle. It is in these disquieting times that exercise can provide much-needed solace.
Research shows that being physically active helps lower cholesterol and blood pressure and can significantly reduce the risk of heart disease, stroke, and diabetes. Physical activity also maintains mass and bone density, reducing the risk of developing osteoporosis (loss of bone density), Sarcopenia (loss of muscle mass), and helps boost one’s immune system, as it flushes bacteria from the lungs and airways, increases white blood cell circulation and raises body temperature, all of which help the body fight infection.
How much Activity is Recommended?
Be active every day, in as many ways as possible. Aim for at least 2 ½ hours of moderate (or 1 ¼ hours of vigorous physical activity) spread throughout the week. The Ministry of Health outlines how much physical activity New Zealanders need to stay healthy https://www.health.govt.nz/your-health/healthy-living/food-activity-and-sleep/physical-activity/how-much-activity-recommended.
Create a Routine
Whether you are looking to maintain an exercise regime or just stay motivated from one day to the next, as your own four walls start to make you feel a bit stir crazy, many people find that it helps to have a set routine. It portions the day into bite-size chunks and allows you to feel a sense of accomplishment as you tick off the day’s tasks.
Few of us are lucky enough to have an exercise bike/treadmill at home. Fortunately, there are plenty of simple exercises that you can do around the house or with household objects that will work instead. If you do not have your own weights at home there are some surprising substitutes you can utilize instead i.e bags of rice or flour, a tin of beans and bottled water can be used, if you need something heavier you can always fill a carrier bag with a few items inside.
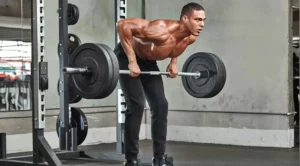
1. Squats
Directions:
Lie on the floor and rest on your back. Ensure that your knees are bent, and your feet are touching the floor.
Put your hands behind your head and then lift both your chest and your legs slightly but leave a gap between them.
Go back to the starting position and repeat.
2. Crunches
Crunches are another important exercise for your abs to strengthen your body core.
Directions:
Widen your feet parallel to your shoulder and extend your arms in front of you.
Bend your knees and your hips slightly and then do the traditional squat position.
Push up using your heels and repeat.
3. Stationary Lunge
Directions:
Stand up straight and put your right leg forwards and your left leg backward. It should look like you’re preparing to run.
Place your hands on your hips. Bend your right leg, leaving a little gap between the floor and the knee.
Then, switch your legs and do the same.
These bodyweight exercises are a great way to start your day and get the blood pumping in your body.
Safety during exercise outside
If you’re working from home, getting outside for physical activity will do wonders for your physical and mental health. Regular walking, running or cycling is a great way to stay active and healthy during lockdown, but it is important to keep your distance and stay more than two metres away from others. Plan your route when you’re thinking of heading out for a cycle/jog. If possible try to think of roads, neighborhoods, and parks that will be quieter and less congested. Follow the latest advice about whether you will also need to wear a mask.
Take a Bit of You Time
Fill your own cup first…Being healthy is not just about maintaining an exercise regime and eating right, it is also about staying mentally healthy too. If you are in isolation with your family, it is easy to spend the day making sure they are happy and entertained, but don’t forget to take a bit of time for you. Do a quick meditation or yoga routine while the kids are watching TV or maybe just go into the garden and take a few deep breaths to relieve some stress!
During this time of uncertainty, something we can take control of is our health and well-being. So, whatever your situation, try to keep active, eat healthily, and stay hydrated.
Ngā mihi and stay safe
Stay connected: Social connection is inevitably limited at the moment but catching up with people via text or facetime will help prevent feelings of isolation.
Maintain some form of routine: Maintaining a routine helps provide some structure do days which often all seem to merge into one.
Get fresh air where possible: Daily fresh air can provide an easy change of scenery when we are stuck at home most of the day.
Gentle exercise is a MUST!
Stay Hydrated: Drinking enough water is important to keep your body hydrated and makes sure your body functions properly.
Eat well- You’d be surprised how your diet can affect how you feel. Gut health in particular is linked to mental health.
Get to that “thing” you’ve been delaying for months
Pick up a good book
Learn new habits or rediscover old ones
These may seem like simple strategies but sometimes it’s the simple things that are most effective