Sciatica Pain
Sciatica is not a diagnosis, it is a term that describes symptoms of pain, pins and needles, numbness and in some cases weakness that radiates along path of the sciatic nerve from the lower back to buttocks and leg.
Causes of Sciatica?
- Disc derangement / herniation
Disc injuries are most common cause of sciatica. Discs are cushion like pads located between each spinal segments that act as shock absorbers. The core interior of the discs is made up a gel like substance called the nucleus pulposus surrounded by thick fibrous outer ring called the annulus. Sudden forces applied to the disc can result in the the core interior to push through the outer ring resulting in a disc bulge or in severe cases can rupture the outer ring resulting in disc herniation which can compress the nerve root. - Disc degeneration / Arthritis / stenosis
Age related degenerative changes in the spine can result thinning of the disc and narrowing of the spinal joints. Overtime the narrowing results in bony growths that can compress the nerve roots resulting in sciatica. - Soft tissue injury resulting in inflammation
Thick ligaments and connective tissue envelope the spinal segments to optimize stability. Injury to any of the structures will result in inflammation and swelling which can affect the sciatic nerve directly resulting in sciatic symptoms. - Piriformis syndrome
Piriformis muscle is a located deep in the buttock region. It originates from the sacrum and inserts into the upper part of the hip. The sciatic nerve travels adjacent to the piriformis muscles. Injury to the muscle resulting in tightness or spasm directly affects the sciatic nerve resulting in symptoms. - Other possible causes:
- Sacroiliac Joint Dysfunction
- Hip joint injury or arthritis
- Spinal fractures
- Tumors
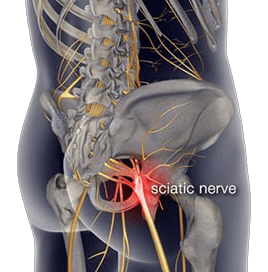
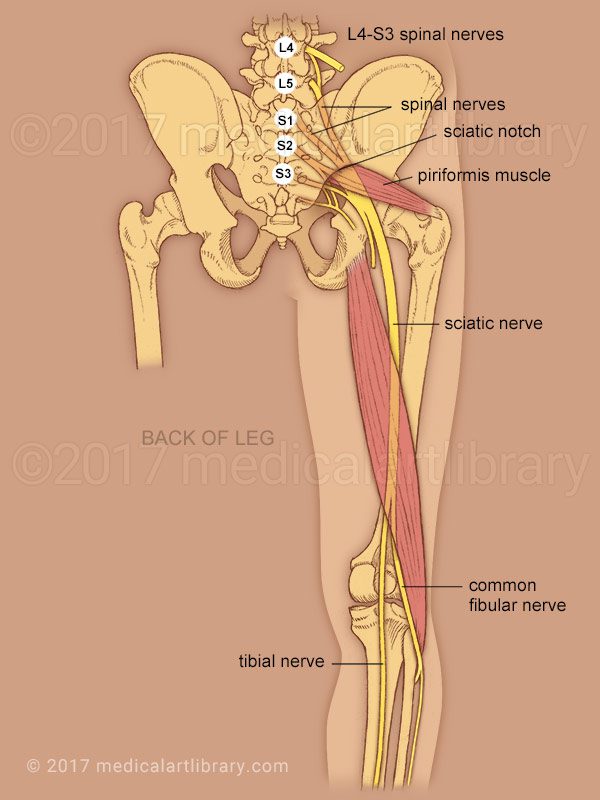
Anatomy of the Sciatic nerve
Sciatic nerve is the largest nerve in the human body. It originates in the lower back from five branches of nerves that extend from the spinal cord. The branches exit the spine at nerve roots L4, L5, S1, S2, S3 connect together to form the sciatic nerve.
The large sciatic nerve then travels deep in gluteal region and descends vertically down to the back of the thigh. It supplies motor function and sensation to the skin and all muscles in the posterior compartment of thigh.
At the knee joint the sciatic nerve then divides into two branches the tibial nerve and common fibular nerve.
What exactly does it feel like?
Symptoms of Sciatica are often characterized by one or more of the following features:
- Unilateral. Sciatica is typically affects one leg.
- Pain. Nature of pain is often constant with heaviness or dull ache. You may experience sharp, shooting, electric shocks intermittently with postural movements.
- Neural irritation. pins and needles with occasional postural numbness is common. Postural numbness can occur when you sit or stand for a period of time, but should resolve with movement. However, if numbness is constant you must be reviewed by your general practitioner or your physiotherapist.
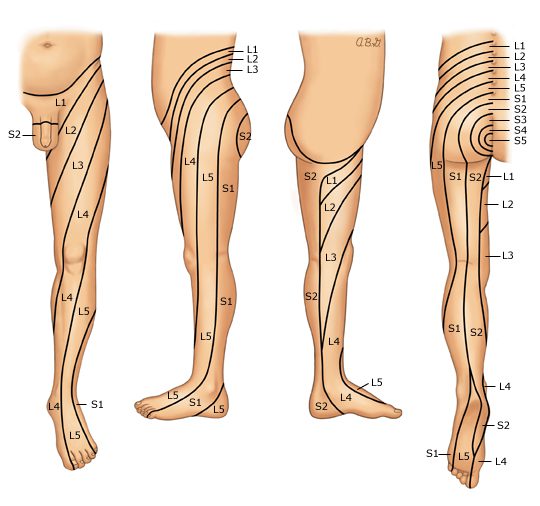
- Location of pain: symptoms of sciatica are felt along the path of the large sciatic nerve. The following picture shows the potential pathways you may feel your symptoms radiate to depending on the origin of nerve irritation or entrapment. Most commonly the areas affected included the lower back, lateral thigh extending to the calf and foot.
If symptoms are presented on both sides with additional symptoms outlined below – this could warrant an urgent medical review.
Red flags
Signs and symptoms that require prompt medical assessment include:
- Age >50 years
- History of trauma
- Severe unrelenting pain that does not resolve with rest or pain control
- Partial or complete loss of bowel and bladder function or control
- Numbness in private regions and the affected side of leg or both
- Discoloration of skin in comparison to unaffected side
- Recent or current infection with fever chills and night sweats
- Sudden unplanned weight-loss
- History of cancer, kidney dysfunction
Diagnosis
It is important to correctly identify the cause your sciatica is essential in order to formulate an effective treatment plan to manage your symptoms and improve function.
Your GP or a physiotherapist will conduct a thorough diagnostic assessment. Your consultation with your clinician will begin with a comprehensive conversion that allows your clinician to formulate an understanding around potential causes of your symptoms. This includes questions specific to your presenting concerns, general health, history of injuries contributing and medication history and your symptoms management strategies. A physical examination is then followed where by your clinician will assess the range of movement of your lower back and lower extremities, reflexes, strength and sensation assessment to test the integrity of the nerve.
Radiographic examination
Further diagnostic examination in forms of radiographic imaging may be recommended by your clinician to assess the quality of your joints, alignment and check for the presence of any potential lesions contributing to your symptoms.
- XRAY – commonly used in initial stages to review underlying joint pathology such as wear and tear of joints, fractures or in some cases to view lesions or tumors
- MRI – high standard imaging that is able to examine in very refined detail possible soft tissues such as muscles, ligaments and internal organs as well as the bony architecture and possible disc injuries.
- Discogram – A discogram test may be helpful in determining abnormalities in an intervertebral disc. A contrast dye injected into the tissues may allow abnormalities in the disc, such as bulging or herniation to be seen on a medical imaging scan (such as computed tomography scan).
Treatment
It is advisable to treat sciatica as early as possible in order to avoid the progression of symptoms. Treatments for sciatica may include both non-surgical and surgical approaches.
Typically, non-surgical management is recommended first. Surgery may be required if non-surgical methods have failed to manage your symptoms or the underlying cause is causing deterioration of symptoms. However, in a few severe cases where red flags are presented, surgery may be considered as the first option
Non-surgical approach is the first step to management. This includes intake of pain medications as prescribed by your doctors and referral to physiotherapy.
Pain medications
Your doctor will prescribe pain medications best suited for your symptoms. These may include
Non-steroidal anti-inflammatory medications such as ibuprofen, celecoxib
Neuropathic medications such as gabapentin, amitriptyline
Analgesics such as codeine, tramadol or oxycodone.
Muscle relaxants such as norflex
Physiotherapy
Physiotherapy will incorporate a combination of gentle strengthening, stretching, and the use of manual therapy to facilitate therapeutic gains.
The goals of physiotherapy for sciatic symptom management includes:
- Strengthen muscles of the spine, core and lower extremities.
- Improve flexibility of any tight muscles
- Improve mobilization of the sciatic nerve
- Facilitate optimal circulation through slight conditioning exercise (walking, swimming)
- Education around activity modifications (especially for work-related participation)
Alternative therapies such as acupuncture may be recommended in combination to physiotherapy to facilitate management of your symptoms.
Acute mild sciatica usually improves with 4 to 6 weeks with regular conservative treatment. However, for moderate to severe cases of sciatica especially with a chronic underlying pathology pain may last over 8 weeks and, treatment time may take longer.
Steroid Injections
Steroid injections are slightly an invasive method used for pain management. Your specialist or an orthopedic surgeon may recommend and administer the injection. In addition to this, injections are also used as a diagnostic method to identify the target nerves or nerve roots affected. The common types of injections for sciatic pain relief include epidural injections.
Surgical approach
In cases where pain and or weakness persists for more than 6-8 weeks or if your symptoms are affecting everyday activities – Surgery may be considered. Your physiotherapist or doctor will arrange the referral for you to meet with an orthopedic back surgeon. Depending on the cause of your sciatica, your surgeon will discuss with you in detail the intended surgical approach, risks involved, post operative management and possible adverse reactions you may have after surgery.