Concussion recovery

What is a concussion?
A concussion is a type of traumatic brain injury caused by a bump, blow, or jolt to the head or by a hit to the body that causes the head and brain to move rapidly back and forth. Rapid movement causes brain tissue to change shape, which can stretch and damage brain cells. This damage also causes chemical and metabolic changes within the brain cells, making it more difficult for cells to function and communicate (concussionfoundation, 2020).
Have you or someone you know had a fall or blow to the head ? If so it’s important to get medically assessed! It is strongly advised that you discontinue any sporting activities, school or work until a trained medical professional has seen you and given you the green light.
Symptoms
The most common signs and symptoms of concussion are:
- Feeling stunned or dazed
- Confusion, e.g. a delay in answering questions
- Headache
- Nausea
- Ringing in the ears
- Dizziness
- Tiredness
- Balance disturbance – Gait, unsteadiness.
- Vision disturbances (double or blurred vision or ‘seeing stars’)
- Memory loss (amnesia) that improves within a few hours.
Medical care should be sought if symptoms worsen or if there are more serious symptoms such as:
- Loss of consciousness, however brief
- Repeated vomiting
- Slurred speech
- Confusion or disorientation
- Convulsions or seizures
- Memory loss, e.g. being unable to remember what happened before or after the concussion
- Changes in mood or behavior, e.g. unusual irritability
- Drowsiness or difficulty staying awake
- A headache that gets worse and does not go away
- Weakness, numbness, or lack of physical co-ordination.
Recovery times:
Recovery from concussion can take up to 6 months. For the majority, symptoms will improve most rapidly within the first 1-3 months. If symptoms are still present after 6 months, these will most likely resolve after one year (SouthernCross, 2018).
Did you know?
Every year, there are 35,000 head injuries in New Zealand (Feigin et al., 2013). Although head concussion is normally associated with sporting injury, almost 80% occur outside of sporting activity (Theadon, 2014).

Is Physiotherapy routine or advised post head concussion?
A study conducted by Van der walt, 2019 extracted clinical service data from a concussion service provider in Dunedin; this was to determine how often their subjects received or were recommended medical input, including physiotherapy. Results show that of the 147 subjects, 80 subjects (54%) received or were advised neck physiotherapy management and 106 cases (72%) received or were advised vestibulo-ocular physiotherapy management. In 59 cases (40%) both neck and vestibulo-ocular physiotherapy were received or recommended.
The findings suggest that recovery post concussion very often requires specific physiotherapy as part of multidisciplinary care. The evidence for the effectiveness of cervico-vestibular rehabilitation post-concussion is very favorable (Schneider et al., 2014).

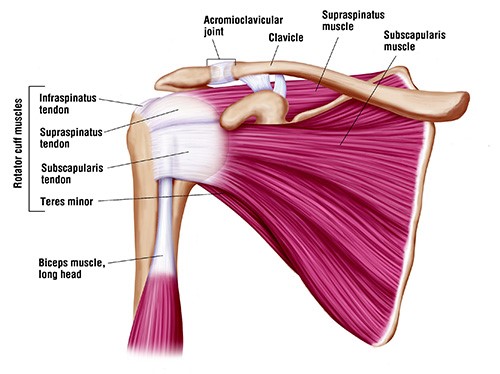
To help get you back on track, your physiotherapist will complete a detailed history of your current complaint/s and medical history. Treatment provided may involve:
- Cervical spine assessment and treatment, including: mobilizations, soft tissue treatment
- Balance assessment and treatment
- Home exercise plan
- Acupuncture
References
concussionfoundation(2020).WHAT IS A CONCUSSION?. Available at: https://concussionfoundation.org/concussion-resources/what-is-concussion. Last accessed 27/08/2020
Southerncross(2018). Concussion – causes, symptoms, treatment. Available: https://www.southerncross.co.nz/group/medical-library/concussion-causes-symptoms-treatment. Last accessed 27/08/2020.
Feigin V, Theadom A, Barker-Collo S et al. Incidence of traumatic brain injury in New Zealand: A population-based study. The Lancet Neurology. 2013;12(1):53-64.
Theadom, A., Parag, V., Dowell, T., McPherson, K., Starkey, N., Barker-Collo, S., and BIONIC Research Group. (2016). Persistent problems 1 year after mild traumatic brain injury: a longitudinal population study in New Zealand. Br J Gen Pract, 66(642), e16-e23.
Van der Walta ,K, Tyson,A, Kennedy, E. (2019). How often is neck and vestibulo-ocular physiotherapy treatment recommended in people with persistent post-concussion symptoms? A retrospective analysis. Musculoskeletal Science and Practice . 39 (130-135), 1-5.
Sport-related concussion: optimizing treatment through evidence-informed practice.J. Orthop. Sports Phys. Ther. 2016; 46: 613-616