Managing your Medial Knee Pain: MCL injuries
What is it?
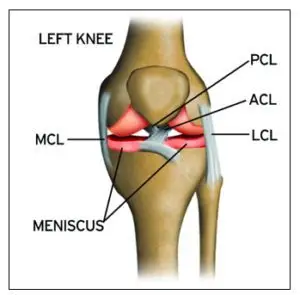
Although your knee has free movement going forwards and backwards, its’ sideward movements are restricted by the robust collateral ligaments on either sides of your knee. The medial collateral ligament (MCL) is situated on the inner part of your knee, but on the outside of your joint. The MCL connects the top of your shinbone (tibia) to the bottom of your femur (thighbone). It helps hold your bones together, provides stability and prevents your knee from bending sideways away from your body.
Injuries to the MCL are from the result of a direct blow to the outer part of your knee- and is most commonly seen in contact sports such as football and soccer. These injures may either over-stretch or cause a tear in the ligament. Whilst surgery may be needed in some severe cases, it is not always the go-to form of management.
Read on to know how physiotherapy can help manage your MCL related-knee pain.
Mechanism of Injury
Injury to the MCL typically occurs when a force drives the lower leg in a sideward direction away from your upper leg and body. Awkwardly landing from a height, twisting of your knee with your foot fixated to the ground, or from a direct blow to the outer part of your knee- most commonly seen in contact sports, are frequent causes of injury to the MCL.
Grading of MCL Injuries
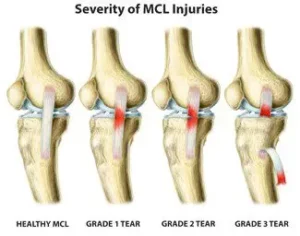
MCL injuries are often graded using the system below:
Grade 1: Regarded as a minor injury- means that the MCL has been overstretched but not torn
Grade 2: Regarded as a moderate injury- means that there is a partial tear in MCL, and presents with some degree of instability in the knee
Grade 3: Regarded as a severe injury- means that the MCL has completely ruptured/torn, and presents with noticeable joint instability
Often 3 MCL injuries are associated with concurrent medial meniscus and ACL ligament damage, which may need surgical intervention. But, the good news is that most MCL injuries may be treated well with conservative physiotherapy management. It usually takes between 2-8 weeks for Grade 1 and 2 MCL injuries to heal, and a graduated rehabilitation programme is highly commended for prevention of future injury.
Signs and Symptoms
Because injury to the MCL may present with similar symptoms as with other knee injuries such as ACL damage, it is vital to have a medical professional such as your physiotherapist evaluate your injury.
Common symptoms of an MCL injury may include:
- Tenderness and pain along in the inner part of your knee
- Swelling in the knee
- Experience catching and locking sensations in the knee joint
- A ‘pop’ sound at the time of injury
- Actual or feeling of giving way of the knee (often indicate grade 2 or 3 injury)
Diagnosis
Your physiotherapist will discuss your injury and its presenting symptoms, past medical history (including a history of any prior knee injuries) and will also undertake a thorough physical examination. During the physical examination, your physiotherapist will assess the structures of your injured knee and compare them to the non-injured side. The range of motion, strength and stability of your knee will be assessed. You may be referred on for imaging such as X-rays and Ultrasounds to help aid the diagnosis. For more severe MCL injuries, and if your symptoms do not resolve with conservative physiotherapy management, you may be referred onto a specialist who may consider referring you for an MRI to get a deeper look at your knee.
Management
The management options for MCL injuries will be dependent on the severity of the injury. In the initial stages of injury, management is focused on controlling swelling and pain, whilst allowing your body to initiate healing processes via inflammation. This is typically achieved through the P.O.L.I.C.E. principles (Protect, Optimal Loading, Ice, Compression and Elevation).
Over the counter medication such as ibuprofen and paracetamol may be taken to reduce pain. Other stronger painkillers and NSAIDs may be prescribed by your doctor to help reduce swelling and inflammation as well.
After assessing your knee, your physiotherapist will frame a rehabilitation programme with exercises tailored to your needs. The purpose of physiotherapy is to help restore your knee’s range of motion, stability and strength, which in turn will then allow you to safely return to your usual day-to-day and sporting activities as soon as possible.
Management of most MCL injuries usually only involves knee bracing and physiotherapy treatment. However, in some cases, surgery may be recommended. Particularly if there is damage to more than one ligament or structure in your knee or if you continue to experience instability in spite of physiotherapy.