Disorders of the Achilles Tendon
Basic Anatomy
The Achilles tendon is the largest tendon in the human-body. It is a band of tissue that connects your calf muscles to your heel bone (calcaneus). This tendon primarily facilitates general mobility such as walking, running, climbing stairs, jumping, and standing on your tip toes, by helping to raise the heel off the ground.
Common Achilles Pathology
Achilles tendinitis and tendinosis are two common disorders and are typically classified as overuse injuries.
Achilles tendonitis involves inflammation of the Achilles tendon. Inflammation is the body’s natural response to injury or disease, and often causes swelling, pain, or irritation. This inflammation is typically short-lived. Over time, if this is left resolved, the condition may progress to degeneration of the tendon- Achilles tendinosis, in which case, the tendon loses its organized structure and is likely to develop microscopic tears.
There are two types of Achilles tendonitis and it is based on which part of the tendon is inflamed:
- Insertional Achilles tendonitis affects the lower portion of your tendon where it attaches to your heel bone.
- Non-insertional Achilles tendonitis involves fibres in the middle portion of the tendon and tends to affect younger people who are active.
In both non-insertional and insertional Achilles tendinitis, damaged tendon fibres may also calcify (harden) and often bone spurs (extra bone growth) develop with insertional Achilles tendinitis. Achilles tendonitis may also increase your risk of sustaining an Achilles tendon rupture (tear).
Causes
Typically referred to as “overuse” conditions, Achilles tendonitis and tendinosis are often caused by the sudden increase in repetitive activity involving the Achilles tendon. This can put too much stress on the tendon too quickly, that can then lead to micro-injury of the tendon fibres. Because of this ongoing stress on the Achilles, the body is not able to repair the injured tissue. The structure of this tendon is then modified, resulting in continued pain and other symptoms. The Achilles tendon also has poor blood supply that makes it more susceptible to injury and may make recovery from injury slow.
Common factors that may lead to the development of disorders of the Achilles tendon include:
- Weak and/or tight calf muscles
- Rapidly increasing the amount or intensity of exercise within a short span of time
- Hill climbing or stair climbing exercises
- Presence of bony spurs in the back of your heel
- Changes in footwear – especially changing from wearing high-heeled shoes to flat shoes
- Wearing poor fitting, inappropriate, or worn out shoes during sporting activities
- Exercising without adequate warm-ups and stretching
- A sudden sharp movement which causes the calf muscles to contract and the stress on the Achilles tendon to be increased. This can cause the tendon fibres to tear.
- Excessive mobility
- Poor feet positioning and biomechanics (excessive pronation and flattening of the arches of the foot)
Symptoms
Common symptoms include:
- Pain and stiffness along the Achilles tendon especially first thing in the morning
- Pain along the tendon or back of the heel that worsens with activity
- Severe pain the day after exercising
- Visible thickening of the tendon
- Tenderness to touch
- Bone spur
- Swelling that is present all the time and gets worse throughout the day with activity
If you have experienced a sudden “pop” in the back of your calf or heel, you may have torn your Achilles tendon. Please seek urgent medical attention if you think you may have torn your tendon.
Diagnosis
If Achilles tendonitis or tendinosis is suspected, please deter from any activity or exercise which causes the pain. It is advisable to see your doctor or physiotherapist as soon as possible so that an accurate diagnosis may be made and appropriate treatment recommended.
You will be asked about the nature and duration of your symptoms and the medical professional assessing you will have a look at your foot and ankle. Ultrasound scanning may be used to evaluate the damage to the tendon and/or surrounding structures.
An MRI may be recommended if symptoms persist. X-rays may also be taken to rule out other disorders which may cause symptoms like Achilles tendonitis and tendinosis.
Treatment
Treatment will depend on the nature, severity, and length of the injury. Generally speaking, the longer the symptoms are present before treatment commences, the longer the timeframe until full recovery is attained. Full recovery may take between three and nine months.
Initial treatment options in the early stages may include:
- Rest – to avoid further injury to the area
- Ice – to reduce inflammation
- Elevation – to reduce swelling
- Non-steroidal anti-inflammatory drugs to reduce pain and inflammation.
How physiotherapy can help:
Physiotherapy typically focuses on two main areas: treatment and rehabilitation. Treatment may entail massage, shockwave therapy, acupuncture, gait re-education, and gentle stretching, whereas, rehabilitation predominantly entails strengthening of the Achilles and surrounding musculature.
Strengthening of the muscles surrounding the Achilles tendon facilitates healing in the tendon itself. Strengthening is attained through the utilization of specific exercises, that will be taught by your physiotherapist. It is common for the rehabilitation programme to take up to three months.
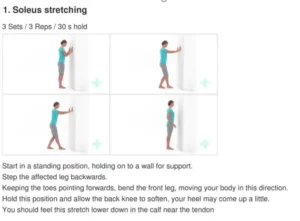
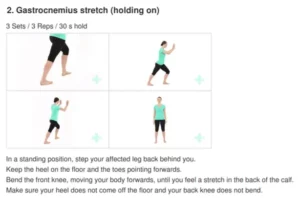
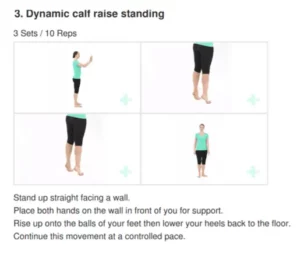
Exercises